Psoriasis
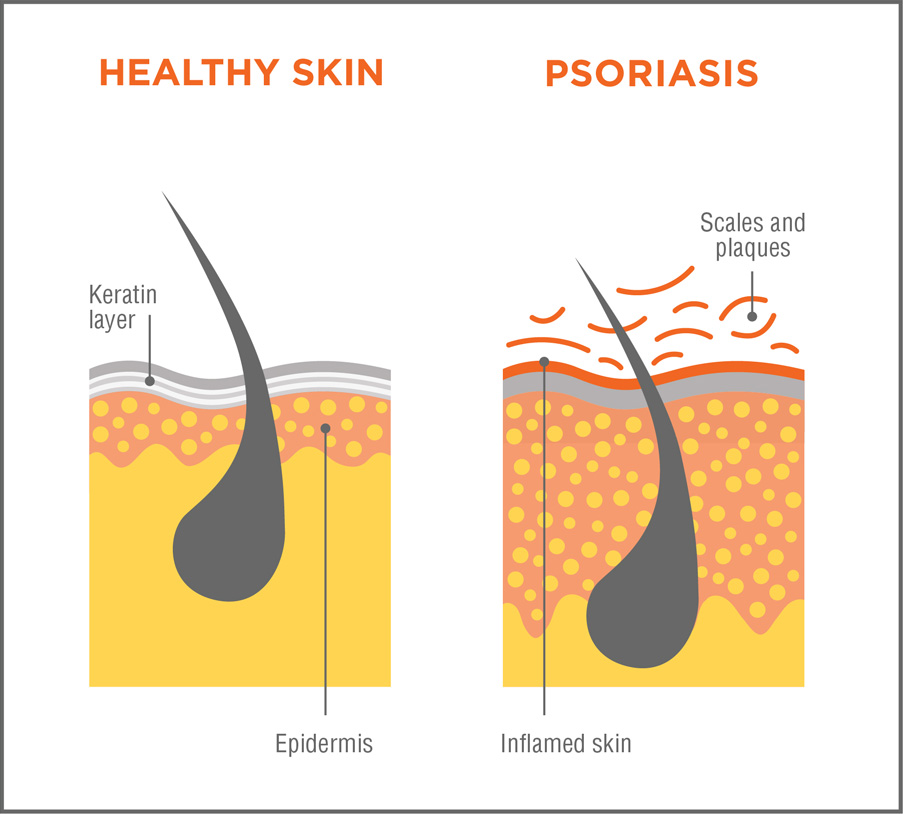
Psoriasis is a common skin condition that can affect anyone, although it’s more common in people between the ages of 15 and 35, according to the National Psoriasis Foundation. If you have psoriasis, your skin cells grow faster than normal. The body naturally develops new skin cells every month to replace skin that sheds or flakes off.
With psoriasis, new skin cells form within days rather than weeks. This rapid growth causes dead skin cells to accumulate on the skin’s surface, resulting in thick patches of red, dry, and itchy skin.
Types of Psoriasis
There are five (5) types of psoriasis that can affect the scalp, nails and joints:
- Plaque Psoriasis – this common form of psoriasis causes raised, red patches on the skin. Skin patches can be itchy and painful;
- Guttate Psoriasis – this type of psoriasis can start in childhood or young adulthood;
- Inverse Psoriasis – this type of psoriasis causes red lesions in body folds;
- Pustular Psoriasis – this type causes white blisters and red skin; and
- Erythrodermic Psoriasis – this rare inflammatory type of psoriasis can develop over the entire body. Symptoms include widespread redness, pain, and severe itching.
Psoriasis Causes
The exact causes of psoriasis are unknown. However, it’s believed that your immune system and genes may contribute to the condition. Your body’s T-cells normally fight viruses and bacteria. In psoriasis, they may start to attack healthy skin cells. Your body increases its production of new skin cells in response to this attack. These new skin cells move to the outer layer of your skin before dead skin cells shed, thus triggering scaly skin patches.
Psoriasis is not contagious. However, the condition may run in families. Risk factors for psoriasis include, but are not limited to, the following:
- family history of the condition;
- viral or bacterial infection;
- obesity;
- smoking;
- uncontrolled stress; and
- use of certain medications such as those used to treat bipolar disorder and high blood pressure.
Psoriasis Complications
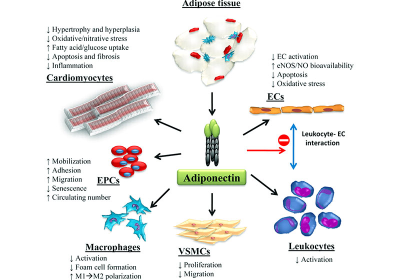
Psoriasis can increase your risk for other illnesses. Some people develop psoriatic arthritis, which can cause severe joint damage. There is also a greater risk of developing type 2 diabetes and cardiovascular disease. Other possible complications of psoriasis include an increased risk for high blood pressure, celiac disease, Crohn’s disease, Parkinson’s disease and kidney disease
Psoriasis can develop anywhere on the body and become a widespread problem. Consequently, you may experience periods of low self-esteem, social isolation, and depression.
Psoriasis Prevention
There’s no way to prevent psoriasis. You can reduce flare-ups by following your doctor’s treatment plan and recommendations and by avoiding common triggers like stress and smoking. Psoriasis is a lifelong condition but it doesn’t have to negatively impact the quality of your life. Talk to your doctor if you have symptoms of psoriasis or if the condition causes depression or mood problems.
Psoriasis Treatments
There’s no cure for psoriasis but, with treatment, you can reduce inflammation and skin irritation. Some treatment options are described below.
Topical therapy – Your doctor may prescribe creams or ointments for your skin or scalp. These can include:
- topical corticosteroids;
- vitamin D;
- analogues topical retinoids;
- salicylic acid; and
- moisturizers
Light therapy – this therapy exposes skin to natural or artificial ultraviolet light under medical supervision. This treatment helps slow the growth of new skin cells.
Medications – If your psoriasis is severe or doesn’t respond to other treatments, your doctor may prescribe medications to suppress your immune system. Along with treatments recommended by your doctor, you can take other steps to reduce symptoms. Oatmeal baths may soothe irritated, red skin. Applying moisturizer to dry, itchy skin immediately after a bath or shower can also reduce flare-ups.
Diet and Stress Management – Psoriasis may also improve if you limit alcohol consumption and learn ways to manage stress.
Discuss your condition and the treatment options above with your doctor to determine the most suitable options.
Tips to treat psoriasis at home:
- Dietary supplements: Fish oil, vitamin D, milk thistle, and evening primrose oil have been reported to help some sufferers. Fish oil applied directly to the skin has also been known to work well for some;
- Use a humidifier to keep the air in your home or office moist;
- No dyes or perfumes;
- Eliminating red meat and fatty foods have been effective for some. The National Psoriasis Foundation lists soy, nuts, chocolate, and cranberries as a few “functional foods” for treatment;
- Applying olive or vegetable oil to scales and patches of psoriasis can lock moisture and nutrients in; and
- Lukewarm baths with Epsom salt, mineral oil, milk, or olive oil can soothe the itching and infiltrate scales and plaques.